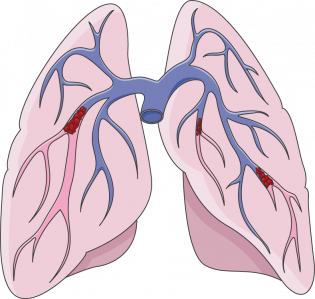
Pulmonary embolism (blood clot in the lungs)
What is a pulmonary embolism?
— Pulmonary embolism (or “PE”) is a blockage in 1 or more of the blood vessels that supply blood to the lungs. Most often these blockages are caused by blood clots that form elsewhere and then travel to the lungs. In rare cases, blockages can also be caused by air bubbles, tiny globs of fat, or pieces of tumor that travel to the lungs.Why are blood clots dangerous?
— If a blood clot forms or gets stuck inside a blood vessel, it can clog the vessel and keep blood from getting where it needs to go. When that happens in the lungs, the lungs can get damaged. Having blocked arteries in the lung can also make it hard to breathe and can even lead to death. Most blood clots in the lungs actually form in the legs or pelvic area (where the legs connect to the body) and then travel to the lungs. Anyone who has had a blood clot in the lungs or who is at risk of a clot should know the symptoms of clots in these areas.What are the symptoms of blood clots in the lungs?
— Common symptoms include:- Panting, shortness of breath, or trouble breathing
- Sharp, knife-like chest pain when you breathe in or strain
- Coughing or coughing up blood
- A rapid heartbeat
What are the symptoms of blood clots in the legs?
— Blood clots in the legs cause different symptoms depending on whether the clots form in veins deep in the leg or in the veins near the surface of the skin. Blood clots in the deep veins of the legs (also called “DVT”) are the most dangerous. Clots in the deep veins can cause:- Swelling
- Pain
- Warmth and redness in the involved leg
Is there a test to find blood clots in the lungs?
— Yes. There are several tests doctors can use to find out if a person has a blood clot in a lung. The most common tests include:- D-dimer blood test – D-dimer is a substance in the blood. The amount of D-dimer often goes up in people with a blood clot in a lung. This blood test is often done together with other tests.
- CT pulmonary angiogram (also called a CT-PA) – A CT pulmonary angiogram is a special kind of X-ray that involves the use of computers. During this test, a dye is injected into 1 of your veins. The dye shows up on X-rays and can show if any blood vessels are blocked.
- A ventilation/perfusion lung scan (also called a V/Q scan) – For this test, you breathe in a small amount of a radioactive substance. You also have a radioactive dye injected into 1 of your veins. Then doctors look at how the different substances look on the scan. The scan can show if 1 of the arteries in the lung is blocked.
- Pulmonary angiography – For this test, you have a small tube called a “catheter” inserted into 1 of the large veins in your body, usually 1 in your leg. Then doctors gently push this tube up into the chest to where the major blood vessels of the lung are found. When the tube is in place, the doctors inject a dye that shows up on an X-ray.
How are blood clots in the lungs treated?
— Blood clots in the lungs are treated with medicines that dissolve clots or that keep clots from getting bigger. Some of these medicines are injected directly into a vein, while others come in shots or pills. Most people being treated for a blood clot in the lung are treated first in the hospital. After being released from the hospital, people who have had clots are usually put on medicines to prevent future blood clots. These medicines are called “anticoagulants,” “blood thinners,” or “anti-clotting medicines.” Almost everyone is put on an anti-clotting medicine that comes in a pill for at least 3 months (and usually longer). Some people are put on an anti-clotting medicine that is injected under the skin, called heparin. This might be for the first few days they are home, or longer if for some reason they can’t take pills. Anti-clotting medicines do not dissolve existing blood clots, but they do keep them from getting bigger. They also help keep new blood clots from forming. Being on an anti-clotting medicine for a few months is important because it gives the body time to dissolve the old clot. It’s also important because people who have a clot are at risk of developing another clot, especially in the first few months. There are a few different anti-clotting medicines that come in pill form. If your doctor puts you on an anti-clotting medicine, take it exactly as directed. If you forget or miss a dose, call your doctor to find out what to do. When you start taking an anti-clotting medicine, you will need to have your blood tested. If you are taking warfarin, you will need regular blood tests to check how your blood is clotting. If there are changes in your medical condition or test results, your doctor might need to adjust your dose. At the wrong dose, the drug can either stop working or lead to serious bleeding. In fact, bleeding is a risk with all the anti-clotting medicines, so you and your doctor should also always watch out for signs of bleeding. People who cannot take medicines to treat clots, or who do not get enough benefit from the medicines, can get a different treatment. This is called an “inferior vena cava filter” (also called an IVC filter). The inferior vena cava is the large vein that carries blood from your legs and the lower half of your body back up to your heart. IVC filters go inside the inferior vena cava. They filter and trap any large clots that form below the location of the filter. Your doctor might suggest 1 of these filters for you if:- You cannot safely take anti-clotting medicine
- You form clots even while on anti-clotting medicine
- You have a dangerous bleeding problem while on anti-clotting medicine
- You are so sick that another pulmonary embolism could kill you
Can I do anything on my own to prevent blood clots?
— Yes. People sometimes form clots because they have been sitting still for too long. People who travel on long airplane flights, for example, are at increased risk of blood clots. Here are some things you can do to help prevent a clot during a long flight:- Stand up and walk around every 1 to 2 hours
- Do not smoke just before your trip
- Wear loose, comfortable clothes
- Shift your position while seated, and move your legs and feet often
- Drink plenty of fluids
- Wear knee-high compression stockings
- Avoid alcohol and medicines that make you sleepy, because they can impair your ability to move around