What is Spirometry, How is it Performed, and What is it Used For
Spirometry is a key diagnostic tool in respiratory medicine, widely used to assess lung function. Whether you’re experiencing shortness of breath, chronic cough, or wheezing, spirometry can help healthcare providers identify underlying respiratory issues. In this article, we’ll explore what spirometry is, how it is performed, and the various conditions it helps diagnose.
What is Spirometry?
Spirometry is a simple and non-invasive test used to measure how much air you can inhale and exhale, and how quickly you can exhale. It evaluates the volume and flow of air in your lungs, providing valuable insights into the functioning of your respiratory system.
The primary goal of spirometry is to assess the presence and severity of conditions that affect breathing. It can detect obstructive and restrictive lung diseases by measuring two main indicators: Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1).
- Forced Vital Capacity (FVC): The total volume of air you can forcefully exhale after taking a deep breath.
- Forced Expiratory Volume in one second (FEV1): The amount of air you can forcefully exhale in the first second of exhalation.
The ratio of FEV1 to FVC is crucial in diagnosing conditions like asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis.
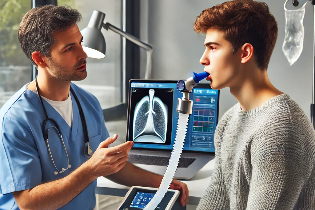
How is Spirometry Performed?
Spirometry is usually performed in a doctor’s office or a pulmonary function testing lab. It’s a straightforward procedure that typically takes about 15 to 30 minutes. Here’s what you can expect during the test:
- Preparation: Before the test, you may be asked to avoid eating a heavy meal or drinking alcohol for a few hours. You may also need to refrain from using inhalers or other respiratory medications, depending on your doctor’s instructions.
- The Test Procedure:
- You will be seated comfortably, and a nose clip will be placed over your nostrils to prevent air from escaping through your nose during the test.
- You will be instructed to take a deep breath in and then blow out as hard and fast as you can into a spirometer (a device that records the air you exhale).
- The test may be repeated multiple times to ensure accuracy. The technician will monitor your effort, and you may be asked to try again if your exhalation isn’t forceful enough or if the test results are inconsistent.
- Post-Test Care: After the test, you can resume normal activities. There are typically no significant side effects, though some people might feel a little lightheaded or tired after exerting themselves during the test.
What is Spirometry Used For?
Spirometry is primarily used for diagnosing and managing lung diseases. It is beneficial in the following situations:
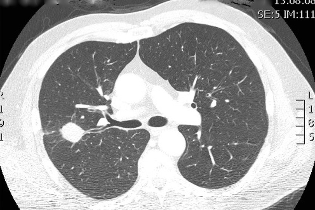
- Diagnosis of Respiratory Conditions:
- Asthma: Spirometry can help confirm a diagnosis of asthma by showing airflow obstruction that improves with bronchodilator medication.
- Chronic Obstructive Pulmonary Disease (COPD): Spirometry is essential for diagnosing COPD, a progressive lung disease that includes emphysema and chronic bronchitis. In COPD, the airflow is obstructed, and spirometry will reveal a reduced FEV1/FVC ratio.
- Pulmonary Fibrosis: This condition causes lung tissue to become stiff and scarred. Spirometry may show reduced lung volumes and impaired airflow.
- Other Lung Diseases: Spirometry can also aid in diagnosing conditions like bronchitis, emphysema, and even lung cancer.
- Monitoring Disease Progression: For patients with chronic respiratory conditions such as asthma or COPD, spirometry is used to track lung function over time. By comparing baseline results with follow-up tests, doctors can assess how well the condition is being managed or if the disease is worsening.
- Evaluating Treatment Effectiveness: If a patient is prescribed a new medication or treatment plan, spirometry can help determine if the treatment is improving lung function. It helps gauge the effectiveness of bronchodilators, inhaled steroids, or other prescribed therapies.
- Preoperative Evaluation: Spirometry is often performed before major surgery, particularly in patients with a history of lung disease. It helps doctors assess the patient’s ability to tolerate anesthesia and recover from surgery.
- Assessing Occupational Lung Conditions: Spirometry can be useful for evaluating lung function in individuals exposed to harmful substances in the workplace, such as dust, chemicals, or asbestos. It helps in detecting occupational lung diseases early.
- Screening for Early Detection: In some cases, spirometry is used for screening individuals at risk of developing lung diseases. For example, smokers over the age of 40 may undergo spirometry to check for early signs of COPD or other lung conditions, even if they aren’t experiencing significant symptoms.
Conclusion
Spirometry is a critical tool in respiratory and sleep medicine, offering invaluable insights into lung function and assisting with the diagnosis and management of a variety of lung diseases. By providing a detailed look at how well the lungs are working, spirometry can help guide treatment decisions, track disease progression, and improve overall patient care. Whether you’re being evaluated for a chronic condition or preparing for surgery, spirometry offers a quick, non-invasive way to assess your respiratory health.