Cough in adults
What is a cough?
— A cough is an important reflex that helps clear out the body’s airways (the trachea and bronchi, which are the tubes that carry air within the lungs). Coughing helps keep people from breathing things into the airways and lungs that could cause problems. It is normal for people to cough once in a while. But sometimes, a cough is a symptom of an illness or condition. Some coughs are called “dry” coughs, because they don’t bring up mucus (phlegm). Other coughs are called “wet” or “productive” coughs, because they do bring up mucus. Some coughs are mild and don’t cause serious problems. Other coughs are severe and can cause trouble breathing.What causes a cough?
— In adults, common causes of a cough include:- An infection of the airways or lungs (such as the common cold)
- Postnasal drip – Postnasal drip is when mucus from the nose drips down or flows along the back of the throat. Postnasal drip can happen when people have:
- A cold
- Allergies
- A sinus infection – The sinuses are hollow areas in the bones of the face that open into the nose .
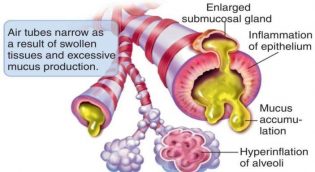
- Lung conditions, like asthma and chronic obstructive pulmonary disease (COPD) – Both of these conditions can make it hard to breathe. COPD is usually caused by smoking.
- Acid reflux – Acid reflux is when the acid that is normally in your stomach backs up into your esophagus (the tube that carries food from your mouth to your stomach).
- A side effect from blood pressure medicines called “ACE inhibitors”
- Smoking cigarettes
Should I call my doctor or nurse?
— Call your doctor or nurse right away if:- You have trouble breathing or noisy breathing (wheezing).
- You have a fever or chest pain.
- You cough up blood, or yellow or green mucus.
- You cough so hard that it makes you vomit.
- Your cough gets worse or lasts longer than 10 days.
- You have a cough and have lost weight without trying.
Will I need tests?
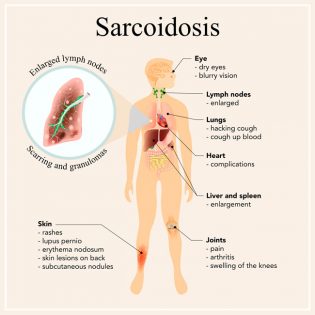
— Maybe. To figure out the cause of your cough, your doctor or nurse will talk with you and do an exam. Based on your symptoms and other factors, he or she might decide that you need tests. These might include:- A chest X-ray
- Breathing tests – Breathing tests involve breathing hard into a tube. These tests show how the lungs are working.
- Allergy skin tests to find out what you’re allergic to – For a skin test, the doctor puts a drop of the substance you might be allergic to on your skin and makes a tiny prick in the skin. Then he or she will watch your skin to see if it gets red and bumpy.
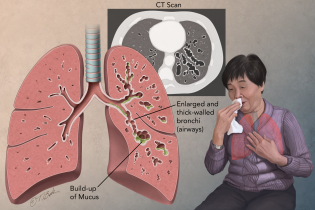
- A CT scan of your chest or sinuses – A CT scan is an imaging test that creates pictures of the inside of the body.
- Lab tests on a sample of the mucus you cough up
- Using a “scope” to look inside your nose, sinuses, airway, or lungs
- Tests to check for acid reflux – These usually involve having a thin tube put in your mouth and down into your esophagus.
Is there anything I can do on my own to get rid of my cough?
— Yes. To help get rid of your cough, you can:- Use a humidifier in your bedroom
- Use an over-the-counter cough medicine, or suck on cough drops or hard candy
- Stop smoking, if you smoke
- If you have allergies, avoid the things you are allergic to (like pollen, dust, animals, or mold)
How is a cough treated?
— Treatment depends on the cause of your cough. For example:- Some infections are treated with antibiotic medicines. If an infection is caused by bacteria, doctors can treat it with antibiotics. If an infection is caused by the flu virus, a different medicine might help. If the infection is caused by another virus (such as the common cold), antibiotics will not help.
- Postnasal drip is treated with different kinds of medicines that can come as a pill or nose spray.
- Asthma and COPD are usually treated with medicines that people breathe into their lungs (called “inhaler medicines”).
- Acid reflux can be treated with medicine to reduce or block stomach acid.
- If you have a cough as a side effect from an ACE inhibitor, your doctor can switch your medicine.