Asbestos exposure
What is asbestos?
— “Asbestos” is the name of a group of minerals that are shaped like long, thin fibers. For many years, asbestos was commonly used in insulation, car brakes, ships, ceiling tiles, fabrics, fireproofing, and many other materials. But since the 1970s, people have mostly stopped using asbestos. That’s because scientists learned that being around asbestos (“asbestos exposure”) can cause serious health problems.
How do people get exposed to asbestos?
— When people are exposed to asbestos, it’s usually because of the type of work they do. Asbestos was used in many types of construction materials. People who worked with these materials in the past might have been exposed to it. This includes plumbers, pipefitters, electricians, insulation workers, construction workers, roofers, welders, and many other types of workers. Also, even though asbestos is no longer used in construction, demolition workers can be exposed when they knock down old buildings.
People can also be exposed to asbestos through the work clothes of someone they live with. This can happen when the person who works with asbestos brings their work clothes home. Plus, people are exposed to low levels of asbestos in nature.
What health problems does asbestos exposure cause?
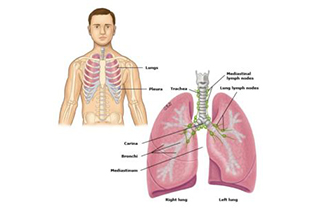
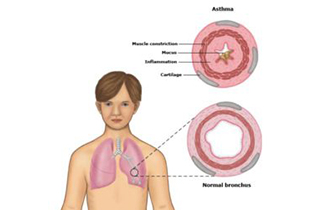
— Asbestos fibers are very small. When these fibers get loose in the air, people can breathe them into the lungs, where they get trapped. The trapped asbestos fibers can cause problems such as:
- Asbestosis – This is scarring of the lungs, which makes it hard to breathe.
- Cancer – This includes lung cancer and “mesothelioma,” a rare cancer that happens in the lining around the lungs or in the belly.
- Pleural problems – These are problems in the thin layer of tissue that surrounds the lungs (called the “pleura”). Asbestos can cause a build-up of fluid in the pleura or scarring. Usually scarring in the pleura does not cause symptoms.
It usually takes being exposed to asbestos at high levels or for a long time for the asbestos to cause illness. Many people who are exposed to asbestos never get sick from it, especially if they don’t smoke.
What are the symptoms of asbestos exposure?
— Many people have no symptoms at all for up to 15 to 30 years after being exposed to asbestos.
The first symptom is usually trouble breathing, which is also called “shortness of breath” or “dyspnea.” At first, the trouble breathing only happens when you are active and goes away when you rest. But as time goes on, it lasts longer, and it gets hard to breathe even when you are resting.
Other symptoms can include chest pain, a cough, and coughing up blood.
Should I see a doctor or nurse?
— Yes. If you have shortness of breath, you should see your doctor or nurse. Tell him or her if you worked in a job that might have exposed you to asbestos. If you have severe shortness of breath with chest pain or nausea or if you cough up blood, you need to go to the hospital. Having those symptoms could mean that your condition is serious.
Will I need tests?
— Yes. First, your doctor or nurse will ask you a lot of questions, especially about the types of work you have done. It is important to find out how long you were around asbestos and how much you were exposed to it. The doctor will also order tests to find out what kind of health problems you might have because of asbestos. These tests could include:
- Chest X-ray – A chest X-ray can show if the lungs are inflating all the way or if there is scarring or an abnormal growth on the lung. It can also show if there is fluid or calcium between the lungs and the ribcage.
- CT scan – A CT scan is like an X-ray but shows a more detailed picture.
- Breathing tests – These tests measure how well your lungs are working. During these tests, you take a deep breath and then blow out as fast and hard as you can into a tube. A machine connected to the tube measures how much air you can blow out of your lungs and how fast you can blow.
- Thoracentesis – If you have fluid around your lung, your doctor might need to take some of the fluid out for testing. This is called a thoracentesis. During this procedure, the doctor uses a needle to take some fluid from around the lungs.
How is asbestos exposure treated?
— Treatment depends on what problems you have from the asbestos exposure:
- Asbestosis – There is no specific treatment for asbestosis. People who have asbestosis might feel better if they do pulmonary rehab. In pulmonary rehab, people learn exercises and ways to breathe that can help ease symptoms. Some people with severe asbestosis need oxygen.
- Cancers – People with lung cancer or mesothelioma might have surgery, chemotherapy, or radiation therapy.
- Pleural problems – The treatment depends on what type of pleural problem you have. For example, if you have fluid around your lungs, your doctor might put in a tube to drain the fluid. If you have inflammation of the pleura but no cancer, you might be treated with an NSAID such as Ibuprofen.
Your doctor will help you decide the best treatment for the type of health problem you have.
Is there anything I can do on my own?
— Yes. If you smoke, the most important thing you can do is STOP SMOKING! It does not matter how long you have smoked or how much you smoke. The problems caused by asbestos exposure get much worse with smoking. Quitting can slow your disease and help you feel better.
It is also important to keep from having any more asbestos exposure. This might mean wearing a mask and special clothing at work or maybe even changing jobs. Talk to your doctor about this to see if your current job might be a source of asbestos.
Get the flu shot every fall, and the pneumonia vaccine at least once. Infections like the flu and pneumonia can be very hard on your lungs. It’s important to try to prevent them.
A cold or the flu can make it harder to breathe. If your shortness of breath or cough gets worse, call your doctor right away.